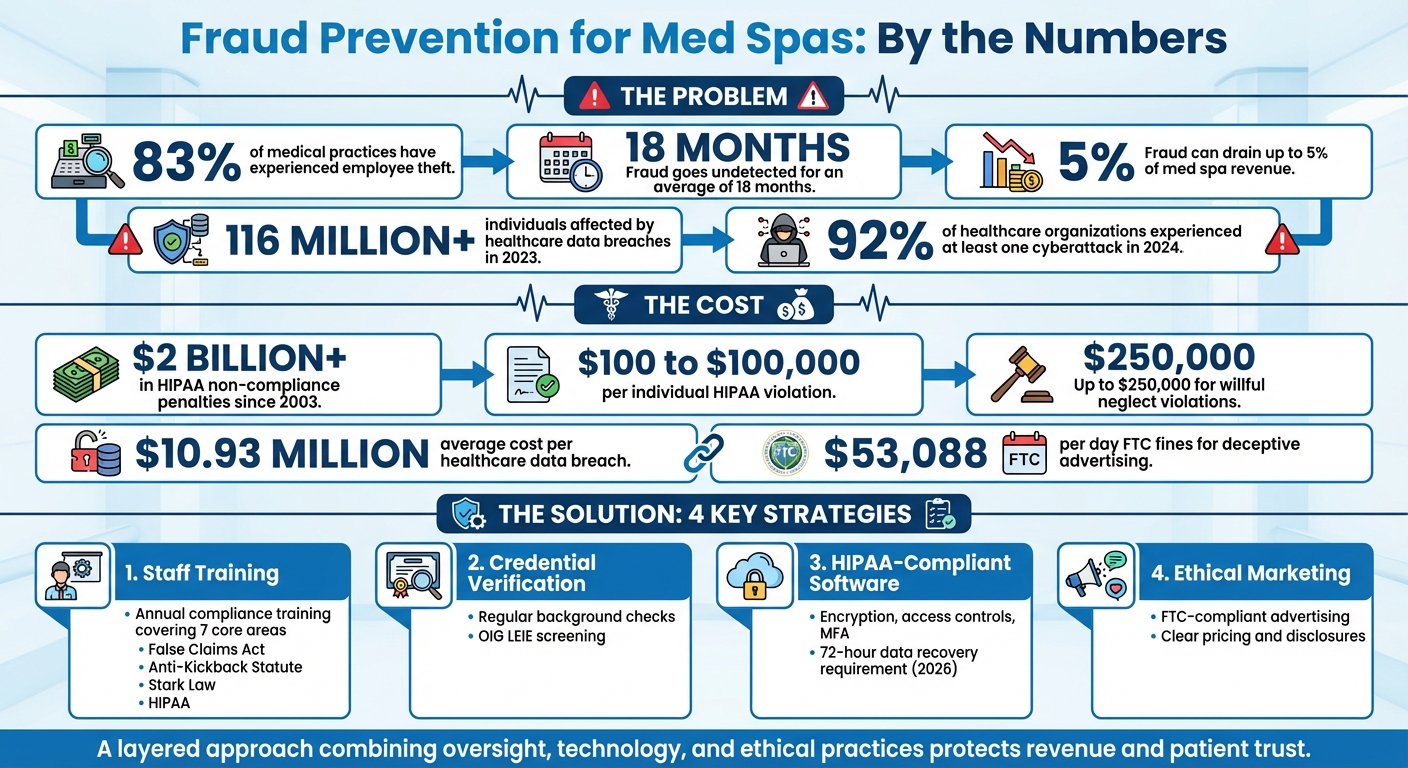
Med spas face serious risks from fraud, which can harm both finances and reputation. Common threats include employee theft, billing fraud, and patient data breaches. Studies show 83% of medical practices have experienced employee theft, and fraud often goes undetected for 18 months. To protect your med spa, focus on these key strategies:
- Staff Training: Teach employees about compliance laws like the False Claims Act and HIPAA. Annual training helps reduce errors and misconduct.
- Credential Verification: Regularly check staff qualifications and run background checks to avoid hiring individuals barred from federal healthcare programs.
- HIPAA-Compliant Software: Use secure systems with encryption, access controls, and multi-factor authentication to protect patient data.
- Ethical Marketing: Follow FTC guidelines for honest advertising and clear pricing to maintain trust and avoid legal issues.
Fraud prevention requires a layered approach combining employee oversight, secure technology, and responsible business practices. By addressing vulnerabilities, med spas can safeguard revenue, comply with regulations, and maintain patient trust.
Med Spa Fraud Prevention Statistics and Key Strategies
Staff Training and Credential Verification
Your employees play a critical role in preventing fraud. With proper training and thorough credential checks, you can build a workplace culture that reduces both intentional misconduct and accidental errors.
Training Staff on Compliance Requirements
Federal regulations, including the Patient Protection and Affordable Care Act, require compliance training for Medicare and Medicaid providers. This training should cover seven core areas: internal monitoring, practice standards, a designated compliance officer, staff training, offense response, open communication, and disciplinary enforcement.
Focus on federal laws that directly impact healthcare providers, such as the False Claims Act, Anti-Kickback Statute, Physician Self-Referral Law (Stark Law), Exclusion Statute, and Civil Monetary Penalties Law. Employees need to understand the consequences of actions like billing for unperformed procedures or allowing unqualified individuals to provide care - both of which can lead to severe penalties.
"A compliance program is a safety net. It establishes strategies to prevent, detect, and resolve conduct that does not conform to federal, state, and private payer health care program requirements, and the practice's own ethical and business policies." - American Academy of Pediatrics
HIPAA training is equally crucial. Common violations include unauthorized access to patient records (e.g., "snooping" into files of friends or celebrities), failure to encrypt data on mobile devices, improper disposal of sensitive records, and disclosing protected health information (PHI) without consent. Without adequate training, these mistakes can result in fines ranging from hundreds to millions of dollars.
Conduct formal training sessions at least once a year and provide additional training when introducing new services, medications, or medical devices. Keep detailed records - such as sign-in sheets and certificates - to demonstrate your commitment to compliance during audits.
Verifying Credentials and Conducting Background Checks
Training alone isn’t enough. Verifying staff credentials and conducting regular background checks are critical steps in maintaining compliance.
Background checks aren’t just about preventing theft - they’re a legal necessity. Under the Exclusion Statute, hiring individuals barred from federal healthcare programs due to past fraud or abuse is prohibited. Regularly check the OIG's List of Excluded Individuals/Entities (LEIE) to confirm that all employees are eligible to participate in federal programs.
"Establishing and following a compliance program will help physicians avoid fraudulent activities and ensure that they are submitting true and accurate claims." - Office of Inspector General (OIG)
Credential verification ensures that only qualified professionals are performing medical procedures. Submitting claims for services provided by uncredentialed staff violates the False Claims Act and can lead to hefty penalties. Assign a compliance officer to oversee credential verification and ensure adherence to standards.
Additionally, conduct regular risk assessments to evaluate staff access levels and address vulnerabilities before they lead to violations. Implement role-based access controls in your patient management system to limit data access based on job responsibilities, reducing the risk of unauthorized PHI disclosure. These proactive measures help identify risks early and strengthen your compliance program.
HIPAA-Compliant Software and Data Security
Your practice management software plays a critical role in protecting against fraud - or, if poorly managed, exposing vulnerabilities. Since 2003, healthcare organizations have faced over $2 billion in penalties for HIPAA non-compliance. Individual violations can range from $100 to $100,000, with willful neglect fines climbing as high as $250,000.
Selecting HIPAA-Compliant Practice Management Software
Choosing software that prioritizes patient data security is essential. One key feature is encryption, which ensures electronic Protected Health Information (ePHI) remains unreadable if intercepted, whether at rest or in transit.
"Encryption is a critical safeguard prescribed by HIPAA laws to protect data from unauthorized access during digital communication or storage." - Sunwave Health
Your software must also enforce strict access controls. For example, a receptionist doesn’t need access to clinical notes. Limiting access to the minimum necessary reduces the risk of internal snooping - one of the most frequent HIPAA violations.
Another crucial feature is automatic audit controls. These track who accessed which patient records and when, creating a digital paper trail that can identify unusual activity early. Without such controls, organizations risk costly breaches. For instance, Gulf Coast Pain Consultants paid $1.1 million in 2024 for HIPAA violations, while Children's Hospital Colorado faced a $500,000 fine for similar failures.
Additional safeguards include automatic logoff after inactivity, integrity controls to prevent unauthorized data changes, and a documented backup plan. The proposed 2026 HIPAA updates will require critical systems and data to be restored within 72 hours following a loss.
"The requirement is that they must have a documented plan to [back up data]. Procedures must be in place." - Invenio IT
Before committing to any software, confirm that the provider will sign a Business Associate Agreement (BAA). Under HIPAA's Omnibus Rule, vendors handling ePHI are considered business associates and share liability for breaches. For example, in 2023, MedEvolve, Inc. was fined $350,000 after failing to secure a File Transfer Protocol (FTP) server, exposing data for 230,572 individuals.
Using Multi-Factor Authentication
While encryption and access controls are vital, adding multi-factor authentication (MFA) provides an extra layer of security. MFA is particularly effective at blocking unauthorized access, even if passwords are compromised.
In 2023 alone, over 116 million individuals were affected by healthcare data breaches, with the average incident costing $10.93 million. Many of these breaches could have been avoided with MFA in place.
"Keep sensitive data under lock and key with passwords that are hard to crack and multi-factor authentication." - Don Silva, Sr., CISO, Raintree Systems
Prepare for the upcoming 2026 HIPAA updates, which will mandate MFA use. Enable it across all platforms managing patient information, including EMR systems, practice management software, email, and cloud storage. Many modern systems now support biometric verification, like fingerprint or face ID, making MFA both secure and convenient for staff on the move.
Current NIST guidelines suggest changing passwords only when a security breach is confirmed or once a year, rather than requiring frequent resets. This approach encourages the creation of longer, more secure passwords, which MFA can then protect. Combine this with annual security training to teach staff how to spot phishing attempts and social engineering tactics.
sbb-itb-02f5876
Ethical Marketing and Advertising Practices
Your external communications play a key role in fraud prevention, just as much as internal controls. Ethical marketing builds trust and helps avoid legal trouble. Misleading advertising can lead to hefty fines, like those imposed by the Federal Trade Commission (FTC), which can reach $53,088 per day, per advertisement for violating cease and desist orders on deceptive practices. Beyond monetary penalties, false advertising undermines trust and makes it harder for patients to make informed decisions about their care.
Following FTC Guidelines
The FTC sets clear expectations: advertising claims must be truthful, non-deceptive, and backed by solid evidence. This applies to both direct claims (e.g., "Treatment X prevents aging") and implied ones (e.g., "Treatment X targets the cells that cause aging").
"An ad is deceptive if it contains a statement - or omits information - that is likely to mislead consumers acting reasonably under the circumstances and is 'material' - that is, important to a consumer's decision to buy or use the product." - Federal Trade Commission
Health claims, such as "clinically proven to reduce wrinkles", must be supported by credible scientific evidence. Similarly, before-and-after photos should reflect typical results, not exaggerated outcomes or digitally altered images. Using these without proper disclaimers is considered deceptive. If testimonials highlight exceptional results, include disclaimers clarifying what the average customer can expect.
Transparency is also crucial in influencer partnerships. Posts featuring paid endorsements or free treatments should include clear disclosures like #ad or #sponsored. Med spas are also accountable for deceptive actions by third-party marketers, such as fake positive reviews.
Disclosures about risks, side effects, or offer conditions must be easy to spot. Avoid hiding them in fine print or using tiny fonts. Instead, place these disclosures prominently and close to the related claims.
Honest pricing is another essential part of ethical advertising.
Clear Pricing and Service Information
Pricing is often a key factor in a customer's decision-making process. Misleading or omitting pricing information can lead to claims of deceptive practices. The FTC's Rule on Unfair or Deceptive Fees, effective May 12, 2025, bans tactics like bait-and-switch pricing or obscuring the total cost of services.
When advertising discounts, ensure the original price is accurate and that the discount reflects genuine savings. If offering a "free" service (e.g., "Buy one, get one free"), don’t inflate the cost of the required purchase or lower its quality. Comparisons to competitor pricing must reflect actual, current prices.
Be cautious with payment models on social couponing platforms, as they may conflict with the Federal Anti-Kickback Statute. When in doubt, consult legal counsel for guidance.
Conclusion
Preventing fraud in med spas isn't about a single solution - it's about creating a layered defense. This means combining human oversight, advanced technology, and centralized management. Key steps like thorough staff training, using HIPAA-compliant systems, and maintaining ethical marketing practices work together to build a strong foundation. By training staff on compliance, separating financial responsibilities, and implementing tools like Prospyr, you can effectively close gaps that might otherwise lead to fraud. This approach directly addresses the "Fraud Triangle" by removing opportunities for dishonest actions.
Fraud can drain up to 5% of a med spa's revenue and often goes unnoticed for as long as 18 months. Even more alarming, 83% of medical practices report incidents of employee theft or embezzlement. These losses don't just hurt financially - they also damage team morale and erode patient trust.
"In the world of health care, trust is everything. Clients trust you with their appearance, health, and self-confidence." - Maven Financial Partners
Prospyr offers the technical tools needed to maintain accountability and prevent fraud over the long term. By integrating CRM, EMR, payment processing, and analytics into one system, it provides centralized oversight of all transactions and patient interactions. This makes it easier to identify mismatches between inventory and sales, detect unusual refund patterns, and keep detailed audit trails that show who accessed information and when. This kind of integration is a cornerstone for effective fraud prevention.
When you combine strong training programs, regular audits, and compliant software, you create a unified system that protects both patient trust and regulatory compliance. With 92% of healthcare organizations experiencing at least one cyberattack in 2024, secure systems and ethical practices aren't just helpful - they're essential. By committing to robust hiring processes, systematic audits, and integrated technology, you're not only preventing fraud but also safeguarding long-term trust and stability. A comprehensive compliance strategy ensures your revenue is secure and your patients' trust remains intact.
FAQs
What types of fraud should med spas watch out for?
Med spas face several fraud risks that can take a toll on their profitability. Some common examples include:
- Embezzlement: Employees misusing or stealing funds.
- Padded invoices: Inflating vendor bills to siphon extra money.
- Pocketed payments: Cash payments taken without being recorded.
Other issues like unauthorized refunds, double billing, and internal theft - often carried out through small, repeated actions - can also go unnoticed for long periods, compounding the problem.
To combat these risks, med spas can adopt strong internal controls, conduct regular audits, and establish clear accountability measures. Additionally, using tools such as AI-powered practice management platforms can improve transparency and streamline processes, reducing the chances of fraud slipping through the cracks.
What steps can med spas take to stay HIPAA-compliant?
Med spas can ensure HIPAA compliance by putting a strong plan in place to protect all forms of protected health information (PHI). Key steps include performing regular risk assessments to spot potential weak points, using role-based access controls to limit who can view sensitive data, and encrypting electronic PHI (ePHI) to keep it secure. On top of that, training staff on privacy protocols is crucial so everyone knows their role in maintaining compliance.
Leveraging a HIPAA-compliant practice management platform, such as Prospyr, makes staying compliant easier. These platforms provide secure tools for patient management, digital intake forms, and communication. Clear policies for handling data, controlling access, and responding to breaches add another layer of protection, helping safeguard patient information while fostering trust.
How does ethical marketing help prevent fraud in med spas?
Ethical marketing is essential for med spas to build trust and transparency with their clients, which is a critical step in preventing fraud. When services, pricing, and expected results are communicated clearly and honestly, it minimizes the chances of misunderstandings or deceptive practices that could result in legal trouble or compliance violations.
By focusing on integrity and adhering to industry standards, med spas can uphold their reputation, stay compliant with regulations, and establish a solid base for long-term success. Beyond fraud prevention, ethical marketing strengthens client confidence and fosters loyalty, ensuring clients feel secure and valued in your practice.



