Laser therapy billing in 2025 requires precise coding and documentation to ensure proper reimbursement and compliance. Here's what you need to know:
-
Key CPT Codes:
- 97037: Low-level laser therapy with provider attendance, reimbursed at $25–$50 per session.
- 0552T: Billed in 15-minute increments, reimbursed at $30–$60 per increment.
- 97039: Unlisted code for high-intensity laser treatments, requiring detailed documentation.
- 17110/17111: For laser destruction of benign lesions.
- 17000–17004: For premalignant lesion destruction.
-
2025 Updates:
- Medicare conversion factor reduced to $32.35, impacting reimbursement rates.
- Therapy cap remains at $3,000 for physical therapy and speech-language pathology, with a separate $3,000 cap for occupational therapy.
- Stricter documentation requirements for unlisted codes like 97039 and 17999.
-
Modifiers and Documentation:
- Use modifier 59 for distinct services and modifier 25 for separate evaluation and management services.
- Detailed records must include laser type, wavelength, treatment area, and medical necessity.
-
Cosmetic vs. Medical:
- Cosmetic procedures (e.g., hair removal, non-ablative resurfacing) are typically self-pay.
- Medical procedures require diagnosis codes and payer-compliant documentation.
-
Technology for Compliance:
- Tools like Prospyr streamline coding, documentation, and billing, helping reduce errors and denials.
Understanding these updates and maintaining accurate records is essential for smooth claims processing and revenue optimization in 2025.
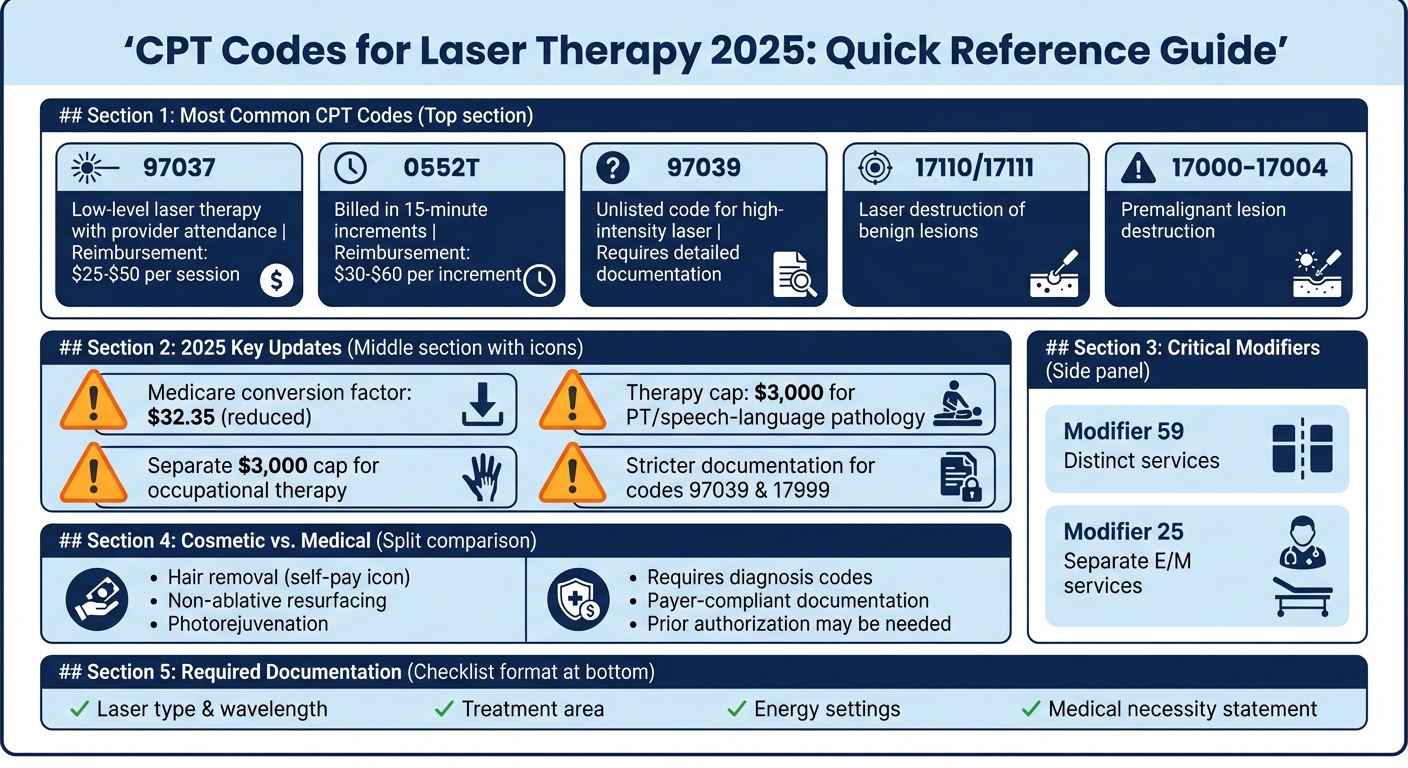
CPT Codes for Laser Therapy 2025: Quick Reference Guide
Common CPT Codes for Laser and Light-Based Therapies
Knowing the right CPT codes for laser procedures is essential for accurate billing. The codes vary depending on whether you’re treating lesions, performing resurfacing, or offering cosmetic services. Each category has its own rules and documentation requirements. Let’s break them down.
Laser Destruction of Lesions
When it comes to laser destruction of skin lesions, the most frequently used codes are 17110 and 17111. Here’s how they work:
- 17110 applies to the destruction of benign lesions (like warts or seborrheic keratoses) for up to 14 lesions in a single session.
- 17111 is used when treating 15 or more lesions in one session.
For premalignant lesions, such as actinic keratoses, use codes 17000–17004. These codes are diagnosis-specific, so your documentation must include the diagnosis, the number and locations of lesions, and details about the laser technique used.
Laser Resurfacing and Skin Rejuvenation
Laser resurfacing doesn’t have specific CPT codes, but practices often use 15780–15783 (originally designed for dermabrasion) for facial resurfacing, depending on the payer’s acceptance. If no specific code applies, you’ll need to use the unlisted code 17999. When using this code, include detailed documentation, such as:
- Laser type and wavelength
- Treatment area
- Energy per cm²
- Number of passes
- Functional impairment being addressed
It’s crucial to distinguish between ablative and nonablative resurfacing. Ablative procedures, like full-face CO₂ laser treatments, remove the epidermis and require thorough documentation. Nonablative lasers and IPL treatments, often considered cosmetic, are generally self-pay services. If the procedure addresses medical concerns, such as post-traumatic scarring or dyspigmentation, ensure your records specify these clinical details.
Cosmetic Laser Procedures
Cosmetic laser treatments, which are typically elective, follow a different billing process. These include services like hair removal, photorejuvenation for sun damage, and pigment reduction. Since these are not covered by insurance, they’re usually handled as cash-pay services using internal practice codes.
For cosmetic procedures without a specific CPT code, you can use the unlisted code 17999. Be sure to include a comparative procedure description to support reimbursement. If you’re dealing with low-level or cold laser treatments for musculoskeletal conditions, 97039 (unlisted modality) might apply, but this also requires detailed documentation.
2025 CPT Code Changes and Compliance Requirements
New and Revised CPT Codes for 2025
Starting January 1, 2025, there will be 270 new CPT codes, 112 deletions, and 38 revisions introduced. While much of the focus is on digital health and AI-assisted services, updates specific to laser therapy remain limited. However, one key change for aesthetic practices involves CPT 97039 (Unlisted Modality). This code now requires significantly more detailed documentation for treatments like low-level laser therapy (LLLT) or cold laser procedures.
When billing under 97039, you’ll need to include specifics such as the laser model and class, wavelength, application site, energy output, treatment duration, and the clinical reasoning behind its use. Thorough documentation can improve claim approvals by 20-30%, while incomplete records risk denials. For dermatologic and cosmetic procedures without designated codes, 17999 (unlisted procedure for skin, mucous membrane, or subcutaneous tissue) remains the standard, and it also demands detailed documentation. These updates highlight the need for improved compliance and meticulous record-keeping.
Updated Documentation and Bundling Rules
Accurate documentation is essential for securing reimbursements and avoiding audits. Practices with high denial rates - 40-50% for 97039 - often fail to include critical details like energy density or evidence of patient progress. To minimize denials, your notes should compare the laser treatment to standard therapies and explain why the unlisted modality was medically necessary.
When using unlisted codes like 97039, bundling them with evaluation codes (97161-97162) requires the -25 modifier. This modifier indicates that a significant and separate evaluation and management service was performed on the same day as the laser procedure. Additionally, it’s crucial to check payer-specific global periods to avoid overbilling issues. Conducting quarterly chart audits can help identify and resolve these problems before they lead to payer disputes. By aligning your workflows with these bundling rules, you can ensure smoother integration with current coding practices.
Current Insurance Policies for Laser Therapy
Medicare and commercial insurers maintain strict distinctions between cosmetic and medically necessary laser services. For procedures deemed medically necessary, insurers increasingly require prior authorization, especially for high-frequency treatments with annual costs exceeding $3,000.
Commercial payers now demand detailed documentation of treatment outcomes and comparative efficacy for laser therapies billed under 97039. Many insurance plans classify both low-level and high-power laser therapies for musculoskeletal and pain conditions as investigational. When billing for laser treatments used to address specific diseases - like vascular lesions or retinopathy - the diagnosis itself, rather than the laser technology, determines the appropriate CPT code and coverage eligibility. Practices that utilize standardized prior authorization forms, including device details and pre-treatment imaging, report a 30% reduction in denial rates.
Best Practices for Laser Therapy Coding and Documentation
Cosmetic vs. Medically Necessary Procedures
When documenting laser procedures, it’s essential to distinguish between cosmetic treatments and those deemed medically necessary, as this impacts billing. Cosmetic laser procedures, like hair removal or non-ablative resurfacing for photoaging, are typically patient-funded. In such cases, use the Z41.1 code and ensure the patient signs a financial responsibility form. For medically necessary treatments, you'll need to use a diagnostic code that reflects the patient's symptoms, functional impairments, or risks. This requires a detailed treatment history, including the condition's onset, duration, and any prior conservative treatments.
Intake notes must clearly state whether the procedure is cosmetic or therapeutic. For medically necessary treatments, include details such as the condition’s onset and duration, prior treatment attempts and their outcomes, and current symptoms like bleeding or pain. Make sure the ICD-10-CM diagnosis aligns with the CPT code and adheres to the payer's medical policies. Be aware that some insurers classify specific low-level laser therapies as investigational and may not cover them, meaning these treatments might need to be self-paid by the patient.
Required Documentation for Laser Procedures
Accurate, thorough documentation is key to selecting the correct CPT code and securing reimbursement. Include the following:
- Diagnosis code
- Lesion details: count, size, location, and whether they are benign or premalignant
- Laser specifics: type, model, wavelength, energy settings (joules/cm²), spot size, pulse duration, treatment time, and number of passes
- Treatment area details: laterality, anesthesia use, and immediate patient response
These specifics are especially critical when using unlisted codes like 97039. Additionally, provide a concise provider note summarizing the medical necessity of the treatment. Clearly differentiate between therapeutic intent and cosmetic improvement, and outline a follow-up plan. If an evaluation and management (E/M) service is performed on the same day, document it separately to justify the use of modifier 25.
How to Use Modifiers and Add-On Codes
Modifiers play a crucial role in billing for laser procedures. Use modifier 25 when the E/M service includes extra history, examination, and medical decision-making beyond the scope of the laser procedure. For instance, if new lesions are evaluated, systemic medications are adjusted, or an unrelated condition (like acne) is addressed during the visit, create a separate E/M note to justify the modifier.
Modifier 59 is used to indicate that a procedure is distinct or separate from other services performed on the same day. For example, if laser destruction is performed on benign lesions of the trunk and a separate treatment is done for a vascular malformation on the face, apply modifier 59. Be sure your documentation specifies the different locations, distinct diagnoses, and clinical indications. Some payers may require more specific modifiers, such as XE, XS, XP, or XU, in place of modifier 59.
Precise lesion counts are essential, as thresholds determine the appropriate code. For bilateral treatments, report units or apply laterality modifiers as needed. If add-on codes are available for “each additional lesion,” bill the correct units based on your detailed documentation of lesion counts and treatment sites.
sbb-itb-02f5876
Using Technology to Improve Laser Therapy Coding
Automated Documentation for Laser Procedures
Aesthetic practices often struggle with selecting the right CPT codes, especially when dealing with unlisted ones like 97039 (unlisted modality) and 17999 (unlisted skin/mucous membrane procedure). On top of that, providing enough clinical detail to satisfy payers can be a challenge. To address this, many practice management platforms now include updated CPT libraries and structured templates. These tools help capture critical data like treatment areas, lesion counts, energy settings, and the medical reasoning behind procedures.
Prospyr's AI-powered note creation and transcription tools take this a step further by converting real-time or recorded provider-patient conversations into structured visit notes. These notes automatically tag key elements such as diagnosis, procedure type, treatment parameters, consent, and post-care instructions. The system aligns these details with CPT documentation requirements. For instance, it ensures that notes clearly differentiate between benign and malignant lesions for codes like 17110/17111 or provide enough detail to support unlisted codes like 97039. It even pre-fills procedure notes and superbills with recommended codes and modifiers, while leaving room for provider review and approval. This not only cuts down on manual data entry but also improves consistency across clinicians, ensuring that documentation meets payers' standards - especially for laser services, which often face scrutiny for potential overuse or cosmetic indications.
When unlisted codes are involved, payers demand detailed descriptions of the procedure, comparisons to standard therapies, and clear justifications for why the service is necessary. Prospyr's AI tool helps by prompting providers to include essential details like the laser model, wavelength, class, parameters (fluence, pulse duration, spot size, total energy), session duration, frequency, total number of sessions planned, prior treatments, and clinical outcomes. This information is then converted into structured documentation ready for payer review, reducing the risk of denials due to incomplete information. In doing so, the system bridges the gap between clinical practice and precise, payer-friendly claims.
Streamlined Workflows for Laser Visits
Integrated scheduling systems now link laser appointments to preset visit lengths, room assignments, and coding templates. Payment tools tied to scheduling and documentation ensure that appropriate service fees are presented - whether for cash-pay cosmetic procedures or for medically necessary treatments requiring copays and pre-authorizations.
Prospyr integrates CRM, EMR, scheduling, and payments, creating a seamless workflow from appointment to billing. The software categorizes appointments as either cosmetic/self-pay or medically necessary/insurance-billable based on diagnosis codes and clinical indications. For medically necessary procedures, the system ensures that ICD-10 codes, medical necessity statements, and proper CPT/HCPCS codes are included. For cosmetic procedures, it defaults to self-pay workflows, customized fee schedules, and financial consent forms, avoiding the accidental submission of non-covered services to insurers. This setup ensures that documentation for medically necessary treatments aligns with payer policies and CPT guidelines, while simplifying workflows for cosmetic services.
"Stop using 7 different systems to manage your practice. With all of your core patient tools in one easy to use place, use your time serving patients." – Prospyr
Monitoring Coding Accuracy with Practice Analytics
Tracking metrics like CPT code usage, denial rates, revenue per visit, and documentation quality is essential for any practice. Analytics can reveal trends, such as providers who frequently use unlisted codes or have an unusual mix of cosmetic versus covered cases, highlighting areas for training or compliance improvements.
Prospyr's practice analytics offer real-time insights into both financial and operational performance. Administrators can investigate problem claims, refine documentation templates, and adjust coding protocols to stay in line with payer policies and CPT updates. The system's automated coding engine reviews documented diagnoses, procedure details, and global periods to suggest appropriate CPT codes and modifiers. It flags inconsistencies - like linking a cosmetic indication to a code typically reserved for medical necessity - and checks for bundling errors or payer-specific rules before claims are submitted. Modifier prompts help avoid errors related to same-day services or global periods.
The platform's CPT library is updated annually to reflect changes - like the 270 new codes, 112 deletions, and 38 revisions introduced in the 2025 release. In-app alerts notify users when updates impact commonly used laser codes or documentation requirements.
Over time, these analytics empower practices to make data-driven decisions about which laser services are the most profitable, which ones need better documentation, and where workflow tweaks can reduce denials. Dr. Daniel Lee, Founder of New Life Cosmetic Surgery, shared that after switching to Prospyr from four separate systems, his practice saw a 50% increase in revenue and a 40% boost in appointments.
Conclusion
The 2025 CPT code set brings 420 updates, including 270 new codes, 112 deletions, and 38 revisions, all effective as of January 1, 2025. For aesthetic practices offering laser and light-based therapies, it’s critical to update fee schedules, EHR templates, and billing workflows to align with these changes. Since many laser services still lack dedicated CPT codes, unlisted options like 97039 (unlisted modality) and 17999 (unlisted skin procedure) remain vital. However, the 2025 guidelines now demand more comprehensive documentation, including details like device class, wavelength, treatment parameters, clinical reasoning, and comparisons to standard treatments.
When selecting codes, focus on the diagnosis and clinical intent rather than the device used. Insurers are placing greater emphasis on medical necessity, so inadequate documentation can result in denials, delays, or lost revenue. It’s also essential to clearly differentiate between cosmetic and medically necessary procedures. Cosmetic cases should follow self-pay pathways, while medical cases require proper diagnosis linkage and detailed records. These challenges also present an opportunity to adopt smarter solutions for compliance and efficiency.
Prospyr offers an integrated platform combining CRM, EMR, scheduling, and AI-driven tools to help practices stay compliant with 2025 CPT guidelines. The system categorizes appointments, embeds CPT-compliant templates, and uses AI to capture critical details like diagnosis, laser settings, treatment areas, and clinical rationale at the point of care. Additionally, its analytics feature tracks code usage, denial trends, and revenue per visit, enabling practices to fine-tune coding protocols and improve staff training. Dr. Daniel Lee of New Life Cosmetic Surgery saw a 50% revenue increase and a 40% rise in appointments after consolidating four systems into Prospyr. This demonstrates how the right technology can simplify compliance, reduce administrative burdens, and safeguard revenue - all while enhancing patient care.
FAQs
What changes to CPT codes for laser therapy should you know about for 2025?
The 2025 updates to CPT codes for laser therapy bring adjustments aimed at refining how these treatments are coded. These revisions are intended to clarify the guidelines for documenting specific laser and light-based procedures, which can play a key role in improving billing accuracy and minimizing the risk of claim denials.
Keeping up with these updates is crucial for securing proper reimbursement and maintaining efficient practice operations. By staying informed and adapting to these changes, you can better align with policy updates and streamline your billing processes effectively.
What documentation is needed to bill unlisted laser therapy codes like 97039?
To bill unlisted laser therapy codes like 97039, you’ll need to provide detailed clinical documentation. This should outline the procedure clearly, including the type of laser therapy used, the specific treatment area, how long the session lasted, and the patient’s response to the treatment.
It’s also crucial to demonstrate medical necessity by including thorough pre- and post-treatment assessments. Keeping accurate and comprehensive records not only ensures proper billing but also minimizes the risk of reimbursement issues. Be sure your documentation adheres to current billing guidelines to streamline the process.
What steps can practices take to comply with the updated CPT codes for laser procedures in 2025?
To keep up with the updated 2025 CPT codes for laser procedures, it's crucial for practices to stay informed about official coding changes and maintain thorough documentation of treatments. Regular staff training on the latest guidelines and conducting periodic audits of coding practices can go a long way in minimizing errors.
A practice management platform, such as Prospyr, can make compliance easier by incorporating CPT updates, simplifying billing, and ensuring accurate coding. These tools not only reduce administrative hassles but also enhance precision, enabling practices to dedicate more time to providing outstanding patient care.