The Centers for Medicare & Medicaid Services (CMS) introduced 130 new billing codes and removed 23 existing ones for 2025. These changes impact aesthetic practices, particularly in billing accuracy, compliance, and revenue management. Key updates include:
- New Codes for Procedures: Skin Cell Suspension Autografts (SCSA) codes (15011–15018) and Laser/Light-Based Therapy codes (96920–96922) now replace unlisted codes, improving billing precision.
- Injectables and Fillers: Updated codes now separate therapeutic uses (e.g., Botox for migraines) from cosmetic uses (e.g., Botox for wrinkles), reducing claim denials.
- Medicare Conversion Factor: Dropped to $32.35 per RVU, a 2.83% decrease from 2024, emphasizing efficient billing practices.
- G2211 Complexity Add-On: Allows additional billing for complex consultations, requiring detailed documentation.
- Telehealth Updates: New virtual care codes (98000–98016) introduced, but Medicare still requires traditional E/M codes with modifiers.
Accurate documentation is essential to avoid claim denials, especially with insurers like Anthem and Cigna increasing scrutiny on codes like Modifier 25. Practices must update workflows and train staff to meet these new requirements.
Key Takeaway: Staying informed about these updates and using tools like integrated billing platforms that support secure payment links can help practices maintain compliance and protect revenue despite reduced reimbursements.
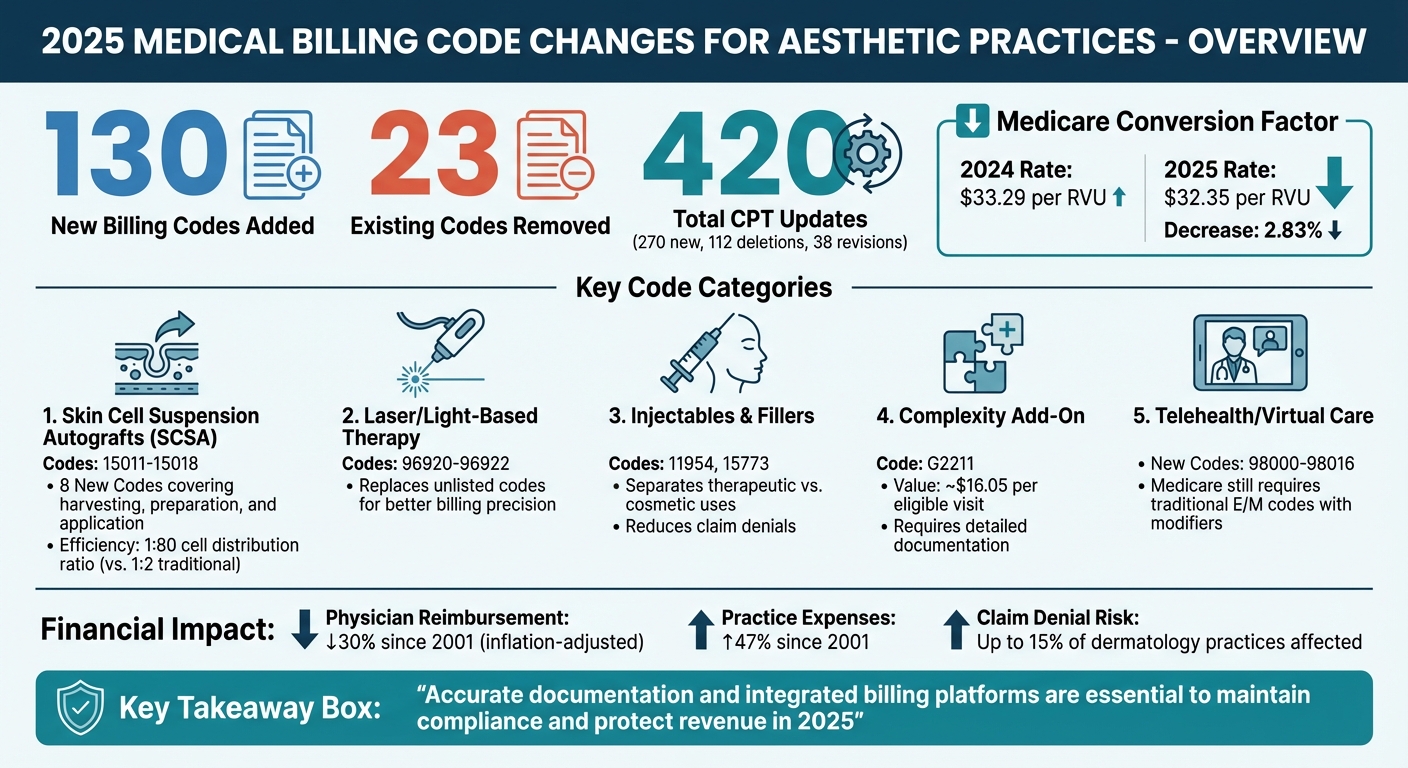
2025 Medical Billing Code Changes for Aesthetic Practices Overview
2025 CPT and HCPCS Code Changes for Aesthetic Practices
The 2025 CPT code set introduces 420 updates, including 270 new codes, 112 deletions, and 38 revisions. Among these, new codes for skin cell suspension autografts (SCSA), laser and light-based therapies, and complex consultations replace unlisted procedures, aiming to improve billing accuracy and reimbursement potential. Leveraging practice analytics can help track these changes and their impact on revenue. Let’s break down the key updates.
Skin Cell Suspension Autografts Codes (15011-15018)
Eight new CPT codes now categorize SCSA into three distinct billable stages: harvesting (15011-15012), preparation (15013-15014), and application (15015-15018). These codes are designed for treatments involving burns, trauma, and skin reconstruction. Unlike traditional grafts, which achieve a 1:2 cell distribution ratio, SCSA delivers a more efficient 1:80 ratio.
For 2025, these contractor-priced codes require meticulous digital documentation to ensure reimbursement. Providers must submit detailed medical records or a charge letter to their Medicare Administrative Contractors (MACs) to justify fees. Some MACs, such as Novitas Solutions and First Coast Service Options, mandate attaching medical records to every SCSA claim. Documentation should include precise square centimeter measurements for both the harvested skin and the application site.
Additionally, while codes 15013-15014 cover manual enzymatic processing, hospital outpatient departments should use HCPCS Level II code C8002 for automated processing.
| CPT Code | Procedure Component | Measurement/Site Criteria |
|---|---|---|
| 15011 | SCSA Harvest | First 25 sq cm or less |
| +15012 | SCSA Harvest | Each additional 25 sq cm |
| 15013 | SCSA Preparation (Manual) | First 25 sq cm of harvested skin |
| +15014 | SCSA Preparation (Manual) | Each additional 25 sq cm |
| 15015 | SCSA Application | Trunk, arms, legs; first 480 sq cm |
| +15016 | SCSA Application | Trunk, arms, legs; each additional 480 sq cm |
| 15017 | SCSA Application | Face, scalp, hands, feet, genitalia; first 480 sq cm |
| +15018 | SCSA Application | Face, scalp, hands, feet, genitalia; each additional 480 sq cm |
Next, let’s dive into the updates for laser and light-based therapy codes.
Laser and Light-Based Therapy Codes (96920-96922)
New CPT codes for laser and light-based therapies address the varying complexities and time involved in treating pigmentation issues, vascular lesions, and skin rejuvenation. These updates replace unlisted procedure codes, which previously required extensive documentation for each claim.
"Properly using these codes can lead to more accurate billing and higher reimbursements, but it's crucial to document thoroughly to justify their use." - Medical Billers and Coders
Add-On and Prolonged Services Codes (G2211, 99417, 99418)
The G2211 complexity add-on code, along with prolonged services codes 99417 and 99418, helps aesthetic practices capture additional time spent on consultations, patient education, and treatment planning.
- Code G2211 applies when managing ongoing complex aesthetic goals or skin conditions.
- Codes 99417 (office) and 99418 (other outpatient) allow billing for every 15-minute increment beyond a standard level 5 E/M visit.
To avoid claim denials, medical records must clearly justify the complexity involved when billing G2211, ensuring proper reimbursement.
sbb-itb-02f5876
Updated Billing Requirements for Injectables, Fillers, and Skin Substitutes
The 2025 updates bring changes to how injectables, fillers, and skin substitutes are billed. One of the most notable updates is the clear distinction between therapeutic and cosmetic applications. For instance, Botox treatments for migraines now require a different code than Botox used for wrinkle reduction.
"The updated codes now separate therapeutic uses (e.g., Botox for migraines) from cosmetic uses (e.g., Botox for wrinkles). Accurate coding ensures you avoid claim denials and get reimbursed correctly." - Medical Billers and Coders
These changes aim to improve billing accuracy for aesthetic procedures. Let's break down the specific coding updates and documentation requirements for injectables, fillers, and skin substitutes.
Injectables and Fillers (11954, 15773)
CPT 11954 is now designated for fillers used on the face and neck. To avoid issues, your documentation must specify the exact anatomic site and the volume used. Similarly, CPT 15773 applies to fat grafting procedures for body contouring. Proper documentation of the site and medical necessity is crucial to prevent claim rejections. Training your staff to differentiate between these codes and using inventory management tools can help reduce billing errors.
Next, let’s look at the updated requirements for skin substitute billing.
Skin Substitute Codes (Q4346-Q4353)
Starting October 1, 2025, CMS introduced a range of HCPCS Level II codes for skin substitutes and dermal matrices, most of which are billed per square centimeter. This includes product-specific codes like A2036 for Cohealyx collagen dermal matrix and Q4383 for Axolotl graft ultra. When billing these products, practices must use JW modifiers to report discarded amounts and JZ modifiers to indicate zero wastage. Reporting wastage is now mandatory for CMS reimbursement and helps minimize claim denials.
Telehealth and Virtual Care Billing Extensions
In 2025, telehealth billing saw updates with the introduction of new virtual care codes for remote consultations, follow-ups, and check-ins. These tools work best when integrated with automated lead capture systems to ensure no patient inquiry is missed. The American Medical Association rolled out a fresh set of telemedicine codes (98000–98016), replacing older telephone codes to better align with how modern practices deliver remote care. These updates offer practices new ways to generate revenue through virtual consultations and follow-ups, as well as brief check-ins.
However, Medicare has not adopted these new codes. Claims submitted with the 98000–98015 series will be denied by Medicare, which requires providers to stick with standard office evaluation and management (E/M) codes (99202–99215) and apply the correct telehealth modifiers. This discrepancy between commercial insurers and Medicare means providers must confirm each payer’s billing policies before submitting claims.
"Medicare has indicated that they will NOT accept the new codes (98000-98015), and all previous guidelines remain in effect, including the required use of office-based E/M codes with the 95 or 93 modifier." - Brad Hart, MBA, MS, CPC, CPMA, COBGC
Medicare’s existing telehealth flexibilities are set to expire on September 30, 2025, unless Congress decides to extend them. Practices must stay vigilant for policy updates and adjust their billing workflows as needed. Below are the specific details of the new code changes.
Virtual Care Codes (98000–98016)
The 2025 updates introduce specialized codes tailored to different types of virtual care. Codes 98000–98007 are designated for synchronous audio-video evaluations, covering both new and established patients, with distinctions based on time spent or complexity of decision-making. Meanwhile, codes 98008–98015 replace the outdated 99441–99443 telephone codes and apply to audio-only visits lasting longer than 10 minutes. For brief virtual check-ins lasting 5–10 minutes with established patients, code 98016 takes the place of the previous HCPCS code G2012.
For Medicare patients who receive audio-only services, providers must use codes 99202–99215 with Modifier 93 and Place of Service (POS) 10 if the patient is home-based. Documentation must indicate that an audio-video option was offered but not utilized. Using POS 10 is essential to secure the higher non-facility reimbursement rate, which generally exceeds the facility rate. When billing commercial payers, practices should confirm whether the new 98000 series has been implemented or if traditional office E/M codes with modifiers are still required before submitting claims.
Implementing 2025 Billing Codes with Prospyr
Adapting to the 130 new codes and 23 removals in 2025 involves much more than just updating a fee schedule. Aesthetic practices must have systems in place to handle documentation requirements, justify complex add-on codes, and manage the financial impact of the 2.83% drop in the Medicare conversion factor - falling from $33.29 to $32.35 per RVU. Prospyr's all-in-one platform tackles these challenges by seamlessly linking clinical workflows with billing operations, ensuring compliance while protecting profitability.
Practice Management Tools for Billing Compliance
Prospyr’s CRM and EMR integration automatically connects clinical documentation to billing records, providing the necessary justification for the new 2025 CPT and HCPCS codes. This is especially helpful for billing the G2211 complexity add-on code, which requires documentation of the ongoing patient-provider relationship. The platform also includes a task management feature to help staff track claim statuses and meet documentation requirements for complex updates, reducing the risk of claim denials.
Prospyr’s analytics and reporting tools are equally important, offering real-time insights into reimbursement trends and coding gaps. With physician reimbursement having dropped 30% since 2001 (adjusted for inflation) and practice expenses up by 47%, these tools are essential for financial stability. The analytics dashboard also helps practices audit billing accuracy, ensuring that new codes - such as Skin Cell Suspension Autografts (15011–15018) and Laser and Light-based therapies (96920–96922) - are correctly applied. These features not only support compliance but also offer opportunities for revenue improvements.
Improving Efficiency and Revenue Growth
Beyond compliance, Prospyr’s tools are designed to boost operational efficiency and revenue. Payment processing and marketing automation features help practices offset Medicare reductions by increasing income from self-pay and cosmetic services. The platform’s AI-powered note creation and transcription tools simplify documentation, making it easier to meet the detailed requirements for Modifier 25 in same-day visits. This is particularly valuable as private insurers like Anthem and Cigna intensify their scrutiny of modifier claims.
Prospyr also integrates AI-driven booking and communication tools, enhancing patient satisfaction while ensuring practices meet new billing requirements. These include telehealth flexibilities extended through 2025, such as audio-only visits and virtual supervision for certain lower-risk services. By addressing these needs, Prospyr enables practices to stay ahead in a changing billing landscape.
Conclusion
The 2025 billing updates bring notable changes for aesthetic practices. These include new specialized codes for laser therapies (96920–96922), skin cell suspension autografts (15011–15018), and the G2211 complexity add-on, which provides an additional payment of about $16.05 per eligible visit. With the Medicare conversion factor set at $32.35 per RVU, ensuring precise reimbursement calculations becomes more important than ever.
Compliance will be a major focus in 2025. Insurers like Anthem and Cigna are ramping up audits on Modifier 25 and the G2211 code, making detailed documentation a necessity to avoid claim denials, which could affect up to 15% of dermatology practices. The shift to Medical Decision-Making (MDM) documentation offers some flexibility, but only if practices have the right systems in place to support it.
To meet these heightened compliance standards and secure proper reimbursements, advanced practice management technology will be indispensable. Platforms like Prospyr provide integrated tools for documentation, compliance tracking, and analytics. With features powered by AI and task management capabilities, Prospyr helps practices manage increased payer scrutiny while capitalizing on new revenue opportunities from self-pay aesthetic services. Given that physician reimbursement has dropped 30% since 2001 (adjusted for inflation), adopting technology that protects profitability is critical for maintaining long-term financial health.
The practices that succeed in 2025 will be those that act promptly - updating their systems, training staff on evolving documentation requirements, and leveraging technology to turn these regulatory changes into opportunities. By staying ahead of the curve, practices can not only navigate these updates but also position themselves for growth in a more complex billing landscape.
FAQs
Which 2025 code changes will impact my aesthetic practice the most?
The upcoming 2025 updates to the CMS billing code structure are set to bring notable changes for aesthetic practices. These adjustments will influence payment rates and outpatient procedures, potentially altering how services are billed. On top of that, new HCPCS codes aimed at managing patients with multiple chronic conditions could reshape billing and reimbursement workflows. These updates aim to refine processes and help ensure payments align with the services provided.
What documentation is required to support G2211 and Modifier 25?
To properly document the medical necessity for both the E/M visit and G2211, your notes should demonstrate the complexity of the visit and highlight the ongoing patient relationship. This is especially important when billing G2211 with Modifier 25 to account for additional services provided during the same visit.
Start by detailing the specific factors that contribute to the complexity of the E/M visit. This might include the patient's medical history, the number of conditions being managed, or any diagnostic challenges. Be sure to outline how these factors required your professional time and expertise.
For G2211, emphasize the continuity of care and the established relationship with the patient. Include details like:
- The patient’s long-term management plan.
- How your care supports ongoing health needs.
- Any adjustments to treatments or follow-ups based on the patient’s evolving condition.
When using Modifier 25, your documentation must clearly separate the additional services from the primary E/M visit. Explain why the extra work was necessary and distinct from the main evaluation, ensuring there’s no overlap between the services billed under each code.
By providing thorough and specific documentation, you can justify the use of both codes, ensuring compliance and accurate billing.
How should we bill telehealth in 2025 for Medicare vs commercial payers?
In 2025, Medicare will require new CPT codes (98000-98016) for billing telehealth E/M services conducted through either audio-video or audio-only communication. When submitting claims, use POS 02 for services provided outside the patient’s home and POS 10 for in-home services, which are reimbursed at the non-facility rate. Medicare will continue to reimburse these services at the same rates as in-person visits. However, commercial insurance plans might have different coverage rules, so it’s essential to check the specific guidelines of each payer.